KENYA LARK PROGRAM
“THE PROBLEM IS EDUCATION: WE HAVE TO TELL THESE LIONS (SICK ADULTS) TO BECOME ANTILOPS (HEATHY HABITS ADULTS) AND THEN, WHEN THEY ARE ANTILOPS, ASK THEM WHAT THEY RESENT OF WHEN THEY WERE LIONS. THIS IS WHAT WE HAVE TO CONVEY”

Optimising linkage and retention to hypertension care and prevention in rural Kenya (LARK hypertension study).
The prevalence of hypertension (high blood pressure) in adults in Africa is the highest in the world.
Lack of linkage and retention to hypertension care and adherence to antihypertensive therapy is associated with increased mortality.
Dr. Fuster, in partnership with AMPATH, is the Principal Investigator of a project in rural western Kenya to assess potential barriers in the management of hypertension.






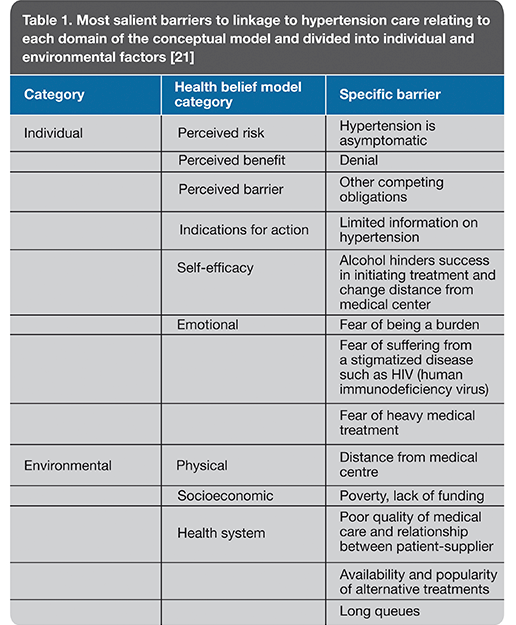
On the basis of the 27 barriers identified which were grouped into individual (cognitive and emotional) and environmental factors, the goal was to develop a tool that would support decision-making and allow to record data for integration into smartphones in partnership with the AMPATH Medical Record System (AMRS). The project also aims to analyse the impact of the use of this tool by community health workers on linkage to hypertension care and management, the reduction (or not) of blood pressure in hypertensive patients, and the cost-effectiveness of the intervention.
Hypertension, the main risk factor for cardiovascular disease is increasing in sub-Saharan Africa, including western Kenya where heart disease is the leading cause of death among people over 30 years old [1, 2]. In rural areas of western Kenya, one in 10 people have high blood pressure ; this high incidence may be due both to traditional causes, such as high salt intake, and more endemic causes, including air pollution caused by burning wood or animal dung for campfires. Further, it is anticipated that by 2025, 75% of all cases of hypertension worldwide will occur in low-medium income countries [3].
The rates of awareness, not to mention treatment and control of blood pressure are low worldwide [4, 5]. In high-income countries, these low rates of treatment and control of hypertension are due to unequal access to healthcare, failure of antihypertensive therapy, comorbidities (such as obesity and diabetes), failure to adopt a healthy lifestyle, poor adherence to medication and other psychosocial factors [4, 6-10]. Low-medium income countries are confronted with all these problems as well as others, such as the lack of a platform for the management of chronic diseases, inadequate access to treatment for cardiovascular diseases, and lack of health human resources (HHR) [11-15].
In the specific case of Kenya, recorded rates of hypertension treatment and control are below 15% and 5%, respectively [16-18]. Given that hypertension can be asymptomatic, linkage and retention to healthcare and adherence to treatment are particularly difficult challenges, and their deficiency is associated with increased mortality [19, 20]. Further issues include the fact that the Kenyan health system struggles to cope with increased demand for healthcare, particularly with respect to non-communicable diseases, rising costs, the lack of facilities and equipment, and the shortage of qualified health professionals. Keep in mind that with only about 1,500 physicians available in the public service, the ratio is of just one doctor per 26,000 population or more [3].
Thus, the first phase of the project carried out by the investigators in rural areas of western Kenya focused on identifying possible barriers to linkage to hypertension care [21]. The study used a qualitative research method based on an analysis of discussions conducted in traditional community assemblies (mabaraza; n=242) and purposive sampling discussion groups (n=169) [21]. A total of 27 barriers to linkage to hypertension care were identified which were grouped into individual (cognitive and emotional) and environmental factors. Cognitive factors included the already mentioned asymptomatic nature of hypertension and limited information on the disease. Emotional factors comprised the fear of being a burden to family or suffering from a stigmatised disease such as HIV. Environmental factors were divided into physical (e.g. distance), socioeconomic (e.g. poverty) and health system-related (e.g. the popularity of alternative therapies, etc.) [21]. This analysis yielded a new methodological approach which may be relevant to studies conducted in other areas in the world with limited resources [21].
The second phase of the NIH-funded project relies on the assumption that the introduction of innovative and effective solutions to address the shortage of skilled health workforce may be a critical component in the management of hypertension. One possible solution to the lack of qualified HHRs would be the redistribution of tasks and management of blood pressure by a team of community health workers [22]. Thus, based on the barriers identified in the first phase of the project, a tool to support decision-making and record data for integration into smartphones will be developed in partnership with the AMPATH Medical Record System(AMRS), involving the conduct of tool usability and feasibility tests by community health workers. A randomised controlled trial will then be conducted to compare the effect of actions carried out by community health workers through standard training vs. a new patient communication strategy based on the use of the tool developed and subsequently integrated into smartphones. The study will evaluate the impact of both strategies on linkage to hypertension care and management (defined as one monthly visit to the clinic, a confirmed visit by a community health worker, or a register of at-home blood pressure readings performed with automatic devices) and on the decrease (or not) in blood pressure in hypertensive patients at one year of follow-up. In addition, a cost-effectiveness analysis will evaluate the costs per unit decrease in blood pressure and the cost per disability-adjusted life-year gained [22]. This study will therefore provide evidence of the efficacy and cost-effectiveness of strategies designed to get patients to start and adhere to hypertension care, which may apply to the management of non-communicable diseases in low-medium income countries [22].
In summary, the programme has made the technology required to measure blood pressure available to part of the Kenyan population; it has trained said population to read blood pressure using these devices and to record it in smartphones. Giving a country with limited resources access to technology lies at the core of this programme thanks to which the best blood pressure register in Africa is now available as a result of the motivation of the people involved. Hypertension in Kenya is now being talked about, and awareness of the risk factors associated with the condition and their prevention has grown as patients are being encouraged to undergo screening tests. All these results encourage us to think that in countries with a medium or low economy, a great deal can be achieved by promoting health initiatives similar to those led by Dr. Fuster.
References
- Gaziano, T., et al., Cardiovascular Disease, in Disease Control Priorities in Developing Countries, D.T. Jamison, et al., Editors. 2006, The International Bank for Reconstruction and Development/The World Bank Group: Washington DC.
- Lewington, S., et al., Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet, 2002. 360(9349): p. 1903-13.
- Fuster, V., et al., Promoting Cardiovascular Health Worldwide: Perspective on the 12 Recommendations from the Institute of Medicine. Scientific American, 2014: p. 1-78.
- Egan, B.M., Y. Zhao, and R.N. Axon, US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA, 2010. 303(20): p. 2043-50.
- Pereira, M., et al., Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens, 2009. 27(5): p. 963-75.
- Cutler, J.A., et al., Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension, 2008. 52(5): p. 818-27.
- Nelson, S.A., et al., Barriers to blood pressure control: a STITCH substudy. J Clin Hypertens (Greenwich), 2011. 13(2): p. 73-80.
- Morgado, M., et al., Predictors of uncontrolled hypertension and antihypertensive medication nonadherence. J Cardiovasc Dis Res, 2010. 1(4): p. 196-202.
- Seedat, Y.K., Impact of poverty on hypertension and cardiovascular disease in sub-Saharan Africa. Cardiovasc J Afr, 2007. 18(5): p. 316-20.
- Wang, P.S., et al., Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med, 2002. 17(7): p. 504-11.
- Samb, B., et al., Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet, 2010. 376(9754): p. 1785-97.
- Kishore, S.P., R. Vedanthan, and V. Fuster, Promoting global cardiovascular health ensuring access to essential cardiovascular medicines in low- and middle-income countries. J Am Coll Cardiol, 2011. 57(20): p. 1980-7.
- Vedanthan, R. and V. Fuster, Urgent need for human resources to promote global cardiovascular health. Nat Rev Cardiol, 2011. 8(2): p. 114-7.
- BeLue, R., et al., An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Global Health, 2009. 5: p. 10.
- Bloomfield, G.S., et al., Chronic noncommunicable cardiovascular and pulmonary disease in sub-Saharan Africa: an academic model for countering the epidemic. Am Heart J, 2011. 161(5): p. 842-7.
- Hendriks, M.E., et al., Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One, 2012. 7(3): p. e32638.
van de Vijver, S.J., et al., Prevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi, Kenya. J Hypertens, 2013. 31(5): p. 1018-24. - Mathenge, W., A. Foster, and H. Kuper, Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population-based survey. BMC Public Health, 2010. 10: p. 569.
- Pastakia, S.D., et al., Screening for diabetes and hypertension in a rural low income setting in western Kenya utilizing home-based and community-based strategies. Global Health, 2013. 9: p. 21.
- Naanyu, V., et al., An exploration of the best location to refer Eldoret and Burnt Forest individuals newly diagnosed with hypertension or diabetes. USAID-Academic Model Providing Access to Healthcare (AMPATH) Program Report, AMPATH, Editor. 2010: Eldoret, Kenya.
Naanyu, V., et al., Barriers Influencing Linkage to Hypertension Care in Kenya: Qualitative Analysis from the LARK Hypertension Study. J Gen Intern Med, 2016. - Vedanthan, R., et al., Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials, 2014. 15: p. 143.


