FAMILY US FAMILIA PROGRAM
“SO THE PROJECT IN HARLEM IS THE TIP OF A LOT OF INFORMATION THAT WE HAVE OBTAINED OVER THE LAST FEW YEARS IN DIFFERENT PARTS OF THE WORLD, AND NOW IT’S GOING TO CRISTALIZE IN THE FAMILY”

The “FAMILIA” Program for the promotion of health in a low-income community in Harlem.
The prevalence of childhood obesity and overweight – factors that significantly increase the risk of cardiovascular diseases – has increased in the United States since the 1960s. A number of health interventions in school children have been carried out in an attempt to deal with this problem. In this context, and based on two previous successful experiences in Spain and Colombia, Dr. Valentín Fuster decided to expand the SI! Comprehensive Health Program (his project for acquiring healthy habits from childhood) to the United States creating the “FAMILIA” Program. The program enrolled 562 children aged 3-5 in 15 of New York City’s preschools and Head Start programs in the high-risk community of Harlem along with 1,000 adults with the aim of demonstrating that education in healthy living habits from an early age reduces the risk of cardiovascular diseases and improves quality of life in adulthood.




Three different research projects were integrated in the program: 1) Evaluation of the cardiovascular health impact of a community-based educational program for the comprehensive promotion of health centered on four areas (eating habits, knowledge of the body and heart, physical activity, and the management of emotions) and targeted to pre-school children and their parents or caregivers; 2) Analysis of multiple lifestyle intervention strategies in adults; and 3) Evaluation of possible genetic changes linked to behavioral changes in children and their parents or caregivers.
Behavioral risk factors such as a lack of physical exercise or unhealthy eating habits significantly increase the risk of cardiovascular diseases, and also the incidence of other risk factors such as overweight or obesity, diabetes, arterial hypertension and dyslipidemia [1]. Some of these risk factors originate in childhood. As an example, children who are overweight or obese are more likely to develop risk factors that can give rise to respiratory, metabolic and cardiovascular disorders [2-6]. The prevalence of childhood obesity and overweight has increased in the United States since the 1960s [7]. The National Health and Nutrition Examination Survey of 2003-2004 showed approximately 17% of all children and adolescents between 2-19 years of age in the United States to be overweight, compared with 14% in the period 1999-2000 [8]. In 1996, in New York City, 20% of the children in the third year of primary education in public and private schools were overweight, versus 21% of the children in the sixth year of primary education [9]. A few years later, in 2003, 43% of the children in primary education in public schools were found to be overweight, and 24% were obese [9]. In this same context, the surveys made among children between 3-5 years of age from low-income neighborhoods in New York also revealed high overweight and obesity estimates (39%) [10-11].
In response to this problem, New York City has launched different initiatives over the last decade, such as the “Eat Well, Play Hard” Program, for the prevention of obesity in childhood through the promotion of positive messages related to healthy physical activity and encouragement of the consumption of fruit, vegetables, and skimmed dairy products. The program also aimed to reduce the number of hours spent by children watching television. According to a 2013 report from the Department of Health and Mental Hygiene of New York City, analyzing data referred to the body mass index of children in public schools from nursery school to the eighth year of primary education (courses 2006-2007 and 2010-2011), the mentioned initiatives were able to lower the prevalence of childhood obesity [12]. However, this decrease was not apparent in the children of Hispanic and Afro-American origin. This circumstance is particularly evident in the area of Harlem in New York, where one of every three children enrolled in the preschool Head Start Program is obese and almost one-half suffer from being overweight or obese.
A number of studies have evaluated the impact of school health education interventions upon health behavior in children [13-20]. Most such interventions were unable to reach the pre-established goals referred to weight loss or the adoption of healthy habits among the children. The main factors underlying this lack of effectiveness include the age of the targeted children (too old: 8 years or older) [16, 17, 21, 22]; the participation of schools with low levels of coordination; the application of programs involving external interviewers and resources (without implication of the school staff); or scant investment in teacher training or the provision of supporting resources.
Considering these limitations [23-25], the experts [26-28] suggest that the prevention of obesity should also involve the community and families. Likewise, it is advisable to focus on realistic interim objectives, such as inducing changes in attitude or acquiring knowledge (e.g., the importance of physical activity and healthy eating habits) as early factors that can result in improved cardiovascular health.
Based on these data, and with the experience of two previously consolidated programs – one in Spain and the other in Colombia – Dr. Valentín Fuster broadened his school intervention project to improve nutritional and lifestyle knowledge, health and habits from childhood (the SI! Comprehensive Health Program) to the United States, through the “FAMILIA” Program in minority communities in Harlem. This program was funded by the American Heart Association with the aim of demonstrating that training in healthy living habits from early ages reduces the risk of suffering cardiovascular diseases and improves quality of life in adulthood. The “FAMILIA” Program was coordinated by Mount Sinai Hospital in New York, in collaboration with the programs of the New York City Administration for Children’s Services (ACS) and the Head Start initiative of the Division of Early Care and Education.
Three different inter-related and synergic research projects were proposed within the “FAMILIA” Program: Project 1) Assessment of impact of a community-based educational intervention designed to promote cardiovascular health from the pre-schooling stage in aspects referred to healthy eating habits, knowledge of the body and heart, physical activity and the management of emotions. The program also had components for teachers and parents or caregivers of these children in order to make their learning environment conducive to positive change; Project 2) Evaluation of the findings of imaging technology and the promotion of health in parents and caregivers; and Project 3) Analysis of how genes couple to increase someone’s risk for cardiovascular diseases and how it sways their lifestyle and behavior.
Project 1:
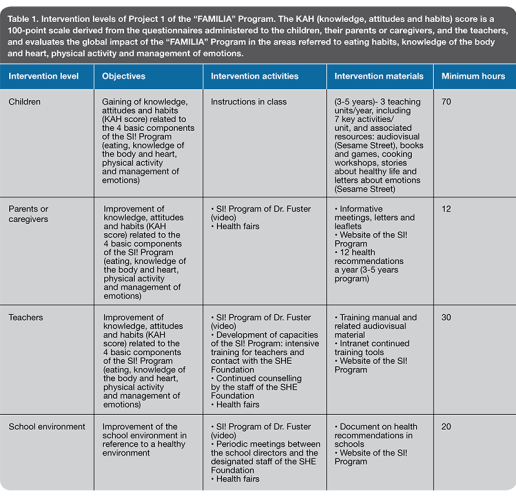
The first project included four levels of intervention: the school’s environment, the teachers, the parents or caregivers, and the pre-school children (Table 1). Questionnaires were used to evaluate prior knowledge among the participants of the body and heart, and their habits and attitudes towards healthy physical activity and foods. Finally, measurements included body weight and height. There were teaching activities for the children in the classrooms, informative sessions targeted to the parents or caregivers, and training programs for the teachers. Subsequently, the acquired knowledge was re-evaluated through interviews with the participants in the program, and body weight and height were measured once again.
Project 2:
The second project involved an intervention program referred to lifestyle among the Head Start parents and caregivers, with an evaluation of the response over time. The study comprised three sections with inclusion of the participants: a discussion group on healthy lifestyle involving 10-15 Head Start parents or caregivers, individual sessions on lifestyle with a personal health coach along with personal fitness monitor device and access to information on health through health fairs or printed educational materials. The impact of these interventions was evaluated using questionnaires with items referred to the level of physical activity, food intake, smoking and quality of life. The impact also was assessed based on physical parameters (height, weight, blood pressure, arterial ultrasound, and blood samples for measuring the glucose, cholesterol and triglyceride levels).
Project 3:
The third project contained in the “FAMILIA” Program in Harlem aimed to explore the following aspects:
Whether some people need additional help (apart from training) to improve their lifestyle and avoid cardiovascular diseases.
Whether genes (DNA fragments responsible for the transmission of hereditary traits) can help find new treatments and methods for preventing cardiovascular diseases.
Whether there are genetic changes linked to changes in lifestyle.
Accordingly, a study analyzed saliva (children) or blood samples (adults). The results of the project 3 are currently being analyzed.
The results of the school-based intervention (project 1) showed that compared with the control group, the mean relative change from baseline in the overall KAH score in children was approximately fold higher in the intervention group (average absolute difference of 2.86 points; 95% confidence interval: 0.58 to 5.14; p = 0.014) [29]. The maximal effect was observed in children who received >75% of the curriculum. Physical activity and body/heart awareness components, and knowledge and attitudes domains, were the main drivers of the effect (p values <0.05). In addition, changes in emotion comprehension trended toward favoring intervened children.
Regarding the project 2, a total of 635 parents/caregivers were enrolled. The mean within-group change in Fuster-BEWAT score from baseline to 12 months was approximately 0.20 points in all groups, with no overall between-group differences [30]. However, high-adherence participants to the intervention exhibited a greater change in the score than their low-adherence counterparts. Furthermore, the knowledge by the participant of the presence of atherosclerosis significantly boosted the intervention effects. Similar results were sustained at 24 months.
Although overall significant differences were not observed between intervention and control groups, the FAMILIA trial highlighted that high adherence rates to lifestyle interventions may improve health outcomes.
This multidimensional school-based educational intervention may be an effective strategy for establishing healthy behaviors among preschoolers and their parents/caregivers from a diverse and socioeconomically disadvantaged community.
References
- Yusuf S et al. Lancet, 2004, 364(9438):937-52. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study.
- Bjorge T et al. Am J Epidemiol, 2008, 168(1):30-7. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents.
- Freedman DS et al. Int J Obes Relat Metab Disord, 2004, 28(1):10-6. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study
- Biro FM and Wien M. Am J Clin Nutr, 2010, 91(5):1499S-1505S. Childhood obesity and adult morbidities
- Duncan GE, Li SM and Zhou XH. Diabetes Care, 2004, 27(10):2438-43. Prevalence and trends of a metabolic syndrome phenotype among U.S. Adolescents, 1999-2000.
- Bibbins-Domingo K et al. N Engl J Med, 2007, 357(23):2371-9. Adolescent overweight and future adult coronary heart disease.
- Ogden CL et al. Adv Data, 2004, (347):1-17. Mean body weight, height, and body mass index, United States 1960-2002.
- National Health and Nutrition Examination Survey (NHANES). 2004.
- Melnik TA et al. Int J Obes Relat Metab Disord, 1998, 22(1):7-13. Overweight school children in New York City: prevalence estimates and characteristics.
- Nelson JA, Carpenter K, and Chiasson MA. Prev Chronic Dis, 2006, 3(2): A49. Diet, activity, and overweight among preschool-age children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
- Sekhobo JP et al. Public Health Rep, 2010, 125(2):218-24. Trends in prevalence of obesity and overweight among children enrolled in the New York State WIC program, 2002-2007.
- Centers for Disease Control and Prevention (CDC). Obesity prevalence among low-income, preschool-aged children–New York City and Los Angeles County, 2003-2011. MMWR Morb Mortal Wkly Rep, 2013, 62(2):17-22.
- Almeida-Pittito B et al. Braz J Med Biol Res, 2010, 43(11):1088-94. Impact of a 2-year intervention program on cardiometabolic profile according to the number of goals achieved.
- Broekhuizen K et al, BMC Public Health, 2010, 10:69. A tailored lifestyle intervention to reduce the cardiovascular disease risk of individuals with Familial Hypercholesterolemia (FH): design of the PRO-FIT randomised controlled trial.
- Castelnuovo G et al. BMC Public Health, 2010, 10:204. TECNOB: study design of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes.
- Foster GD et al. N Engl J Med, 2010, 363(5):443-53. A school-based intervention for diabetes risk reduction.
- Ritchie, LD et al. Trials, 2010, 11:60. Taking Action Together: a YMCA-based protocol to prevent type-2 diabetes in high-BMI inner-city African American children.
- Draper CE et al. BMC Public Health, 2010, 10:398. HealthKick: a nutrition and physical activity intervention for primary schools in low-income settings.
- Galvez MP et al, Acad Pediatr, 2009, 9(5):339-43. Childhood obesity and neighborhood food-store availability in an inner-city community.
- Shah P et al. Br J Nutr, 2010, 104(3):427-36. Improvement in nutrition-related knowledge and behaviour of urban Asian Indian school children: findings from the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ ( MARG) intervention study.
- Stone EJ et al. Prev Med, 2003, 37(6 Pt 2):S13-23. Design, implementation, and quality control in the Pathways American-Indian multicenter trial.
- Caballero B et al. Am J Clin Nutr, 2003, 78(5):1030-8. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren.
- Kropski JA, Keckley PH and Jensen GL. Obesity (Silver Spring), 2008, 16(5):1009-18. School-based obesity prevention programs: an evidence-based review.
- Birch LL and Ventura AK. Int J Obes (Lond), 2009, 33 Suppl 1:S74-81. Preventing childhood obesity: what works?
- Summerbell CD et al. Cochrane Database Syst Rev, 2005(3):CD001871. Interventions for preventing obesity in children.
- Committee on Progress in Preventing Childhood Obesity. 2006, Institute of Medicine of the National Academies. Progress in preventing childhood obesity: How do we measure up?
- USDoHaH S., National Institute of Health: Bethesda, 2004. Strategic Plan for NIH obesity research: a report of the NIH Obesity Task Force.
- Katz DL et al. Int J Obes (Lond), 2008, 32(12):1780-9. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis.
- Fernandez-Jimenez R, Fuster V et al. J Am Coll Cardiol, 2019, 73(16):2011-2021. Child health promotion in underserved communities: The FAMILIA Trial.
- Fernández-Jiménez R, Fuster V et al. J Am Coll Cardiol, 2020, 75: 1 (42-56). Different lifestyle interventions in adults from underserved communities. The FAMILIA Trial.


